Endometriosis; The Career Woman’s Disease?
I have a dear friend who is an acupuncturist. While sticking needles into me in an attempt to reduce my endometriosis symptoms, she shared that when studying endometriosis, it was referred to as the ‘Career Woman’s Disease’ because it has been associated with delayed childbearing. For many years, it was believed to afflict women who delay marriage and pregnancy to pursue careers.
My endometriosis symptoms started when I was a teenager, which is not uncommon, so debunks that myth. It could be more accurate to call endometriosis a career-breaking disease, because it often impacts women’s ability to work for extended and recurring periods of time. However, hearing this sparked my curiosity in the medical history of the disease, which ended up more shocking than finding it defined as the body’s punishment for prioritizing career and independence over creating a family.
Before being labelled the ‘Career Woman’s Disease’, women complaining of symptoms typical of endometriosis were dismissed and often misdiagnosed with Hysteria.
There is a strong case to support the argument that hysteria was never a separate condition, but the term used to describe uncontrollably, emotionally distraught women with ‘delusional’ pain that medical professionals at that time didn’t understand.
“While it is thought of as a modern condition, it has been suggested that endometriosis may have existed for as long as 2,500 years due to descriptions of Hippocratic doctors treating women with chronic pelvic pain. Links have been made between endometriosis and historical descriptions of hysteria (i.e. ideas about behavioral disturbances believed to be caused by the uterus) which, it has been argued, may have been undiagnosed cases of endometriosis. Due to hysteria’s constructions of women as unstable, gender deviant, and unable to bear children, a number of authors have suggested that endometriosis and hysteria share common underlying sociohistorical discourses.” Reference
Nezhat et al. suggests that if it is true that hysteria could represent undiagnosed cases of endometriosis, ‘this would constitute one of the most colossal mass misdiagnoses in human history, one that over the centuries has subjected women to murder, madhouses and lives of unremitting physical, social and psychological pain.” Reference
Medical gaslighting of female health problems is still shockingly common. On average, it takes 8 years for someone to be diagnosed with endometriosis, generally because on average, it takes 8 years of persistent visits before medical professionals take their symptoms seriously.
From the onset of symptoms, it took 10 years before I received an endometriosis diagnosis. By that time, it had developed into stage 4 - the most intrusive stage - creating serious abrasion to multiple organs and a cystic growth on one ovary which, if left, had the potential to become cancerous, leaving me debilitated and basically bed-bound until my saint of a surgeon directed immediate treatment and surgery.
But let’s rewind. After years of doctor appointments that left me questioning my own sanity and integrity, suggesting the pain was all in my head, I started to dismiss it myself. I adopted a soldier-on attitude until my symptoms escalated to the point where I couldn't hide it anymore — female hormones don’t respond well to the chronic stress caused by soldiering on, especially when it involves pushing through shocking levels of persistent pain.
Finally receiving confirmation that I was not crazy, nor responsible for my pain — I had a real, insidious disease — sent me into a spiral of emotion.
First; anger.
Then grief.
I had allowed the lack of external validation of my symptoms to determine my own relationship with my body. I spent years feeling an undercurrent shame for being weak-bodied and not knowing why and pushed myself harder than anyone around me to prove to myself that I was not weak.
With that said, I don’t hold contempt for the medical system. Endometriosis tissue can be difficult to detect, and the hormonal influence on symptoms can be complicated to manage. But the physiological repercussions of professionals not taking patients' pain seriously can perpetuate a situation that is already challenging enough to navigate. Presently, there is no cure and limited treatment options, which each have their own set of adverse side-effects. And the cause is still unknown.
But while it is an inaccurate causal explanation, there may be some merit in the link between neglecting, not necessarily a maternal role, but our own female biology and the development of this disease.
Have you ever heard the saying;
Nature always wins.
It’s a dangerous game; to deny our nature. And our biology is part of our nature. Our gender does not define us — As Walt Whitman was famously quoted;
We contain multitues.
But it is a considerable determinant of how we function in the world. And the bill always comes. The decisions, and behavioural and psychological patterns we support today will bill us tomorrow. And the chronic stress that occurs from trying to keep up with the demands of the modern world and being a ‘Career Woman’ does not always support healthy female hormone function.
Hormonal imbalances are the environments in which diseases like endometriosis flourish.
Endometriosis is a complex inflammatory, estrogen-dominant disease. It has been compared by researchers to cancer in the way it creates its own blood and estrogen supply, which creates a vicious cycle that makes it challenging to control estrogen dominance once it has begun to spread.
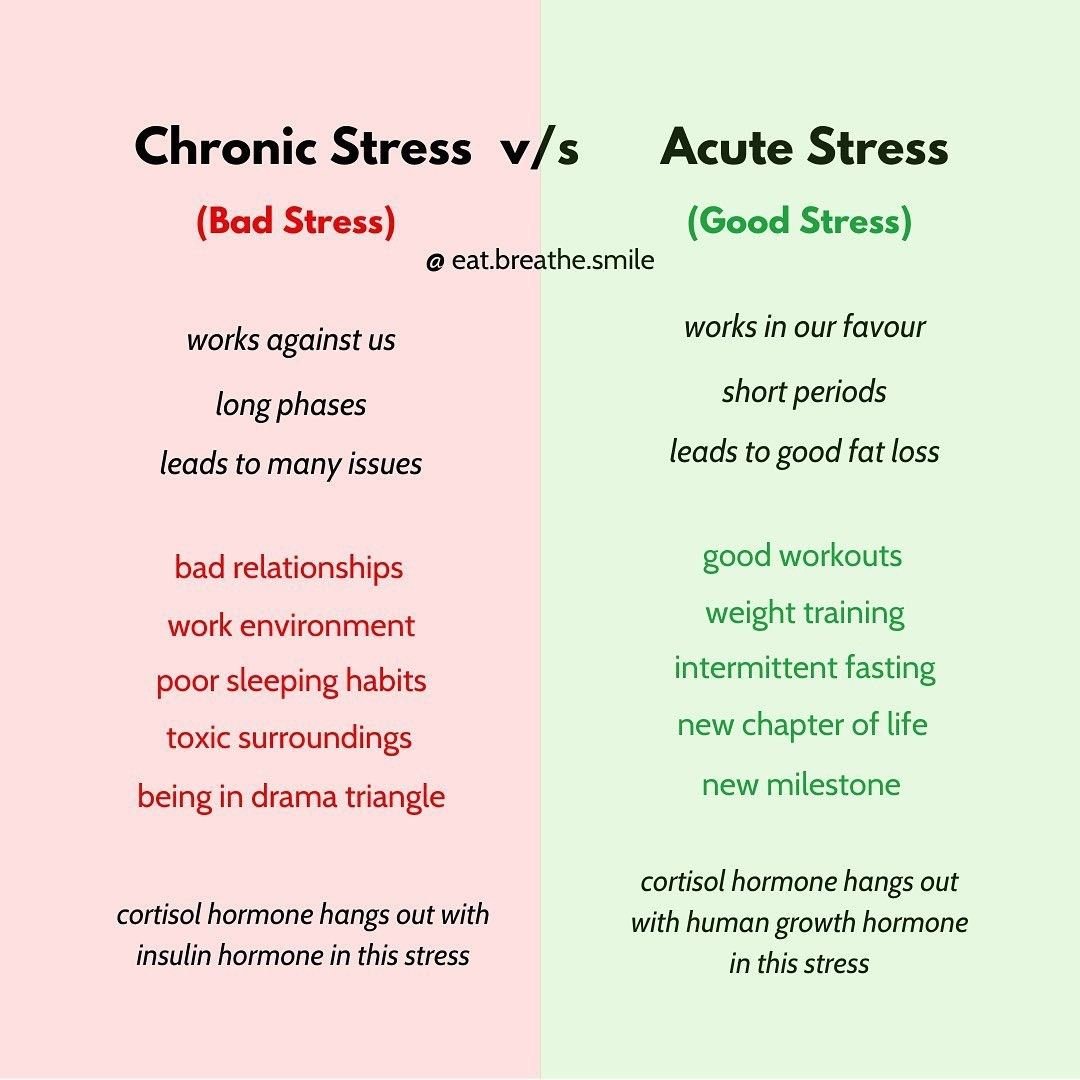
Estrogen dominance can occur for a number of reasons, but one of the most common is chronically elevated cortisol, if not diet, pesticides, over-use of plastics, and heavy metal exposure. The word chronic here is important, because there is a distinction between acute, short-term stress and ongoing elevated cortisol. The first is adaptive, the second; maladaptive, which can occur from physical stress, work, life or time pressure, or an over-active nervous system, overstimulated namely by fear or anxiety. Acute, and particularly, ongoing trauma can also trigger a fight or flight response that can trap the body in a state of stress, and cause pain loops that have been linked to endometriosis.
Back to estrogen.
Dr Mindy Peltz calls the first ten days of a woman’s menstrual cycle, when estrogen rises to its peak, the power phase. A high-energy, high-drive lifestyle supports this phase. But if we try to push that momentum through to the end of the cycle, estrogen can, from my understanding, continue to build and dominate over progesterone.
Progesterone — the hormone that governs the second half of the menstrual cycle — has been proven to limit and sometimes stop the growth of endometriosis tissue outside of the uterus. It is the hormone used for hormone therapy treatments of endometriosis to do just that. (The hormone sourced for hormone therapy, however, is often synthetically produced progesterone, not bio-identical to human progesterone, which can lead to adverse side-effects that all should monitor themselves for while experimenting with this treatment options.)
Opposite to estrogen, progesterone needs rest and restoration for the body to organically produce. It loves nature’s carbs and can be quickly depleted by extreme physical output, diets, fasting, and excessive work.
If we do not allow ourselves to slow down, nourish and nurture ourselves in the sencond half of the mentrual cycle, Progestorone can plummet, leaving excess estrogen to promote the continued growth of endometriosis.
I’m going to take a moment to go right back to high school basics for a moment for those who don’t understand or recall the precise hormonal fluctuations that occur each month and the physical and emotional responses.
Menstrual Phase (Days 1-5):
Hormones: During this phase, levels of estrogen and progesterone, two key female hormones, are low.
Uterine Lining: The shedding of the uterine lining, known as menstruation, occurs. This is triggered by the drop in hormone levels and lasts around 3 to 7 days.
Physically: Some females may experience symptoms such as cramping, bloating, fatigue, and headaches during menstruation.
Emotionally: Mood swings, irritability, and sadness are common during this phase due to the hormonal dip and discomfort associated with menstruation.
2. Follicular Phase (Days 1-13):
Hormones: As menstruation ends, the body begins to prepare for ovulation. Estrogen levels gradually rise, which stimulates the thickening of the uterine lining.
Follicle-Stimulating Hormone (FSH): This hormone is released by the pituitary gland and stimulates the growth of follicles in the ovaries, each containing an egg.
Ovulation: Around the middle of the cycle, typically on day 14 in a 28-day cycle, a surge in luteinizing hormone (LH) triggers the release of a mature egg from one of the ovaries. This is known as ovulation.
Physically: Symptoms of menstruation typically subside, and energy levels may increase as estrogen levels rise. Some females may experience increased libido.
Emotionally: Many females feel more energetic, positive, and social during this phase. However, some may still experience mild mood changes or irritability.
3. Ovulatory Phase (Day 14):
Hormones: Estrogen levels peak just before ovulation, which triggers the release of LH.
Egg Release: The mature egg is released from the ovary and moves into the fallopian tube, where it may be fertilized by sperm if intercourse occurs.
Physically: Some females may experience mild abdominal discomfort or bloating around ovulation. Libido tends to peak due to the surge in estrogen.
Emotionally: Many females report feeling more confident, outgoing, and sexually aroused during ovulation. However, some may also experience heightened emotional sensitivity or anxiety.
4. Luteal Phase (Days 15-28):
Hormones: After ovulation, the empty follicle in the ovary transforms into a structure called the corpus luteum, which produces progesterone.
Progesterone: This hormone helps maintain the thickened uterine lining in preparation for a potential pregnancy.
Menstruation (If No Pregnancy): If the egg is not fertilized and does not implant in the uterus, hormone levels drop towards the end of the cycle. This leads to the breakdown of the uterine lining, and menstruation begins again.
Physically: Symptoms such as breast tenderness, bloating, and fatigue may return as progesterone levels rise. Some females may also experience food cravings or digestive issues.
Emotionally: Mood swings, irritability, anxiety, or sadness are common during the luteal phase, especially in the days leading up to menstruation. This is often referred to as premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD) in more severe cases.
When I took the time to better understand the nuances of these changes and the lifestyle and dietary requirements that support each phase, it was no surprise to me that I had a dominance of estrogens and severe progesterone deficiency — as revealed by a comprehensive DUTH hormone test — which was, undoubtedly contributing to the severity of my endometriosis symptoms.
I could be labeled a career woman. I do not represent every woman with endometriosis, but with stress at the helm of many of the most violent cases, it may be worth considering how your career drive, long-term stress, or neglect of the body’s need for rest may be impacting yours.
This year, the recorded ratio of women with endometriosis shifted from 1 in 10, to 1 in 7.
The rate of childlessness in women is also historically high and rising. “About 1 in 4 Australian women will remain childless by the end of their reproductive lives.” Resource. This indicates that women are choosing to revolve their lives around other things; careers, travel, and freedom from the ‘burden’ of domestic life. I am only speculating here, but the rise in endometriosis seems like an interesting link. There are also more toxins and chemicals in our environment, and more female cycles are being disrupted by the contraceptive pill. The list of possible contributing factors goes on. But the pressure of the modern world on women is also relatively new.
Until I stopped to examine my life, I would never have called myself stressed. I felt pressure but was not overwhelmed by it. My days were full — predominantly full of things I am passionate about — and very active. I had perceived stress as an emotional and mental response to pressure and did not consider high levels of daily physical endurance over a long period of time without balancing it with adequate rest, as stress.
In my youth, I also did not consider the significance of the biological differences between the sexes — gender equality was highlighted in my school. I had high expectations of myself to achieve, build my own life, and create independence and financial freedom, because I believed that that is what a modern woman must do to survive.
But the ‘tenacity’ and ‘discipline’ I embraced through-out my early 20s caused me to ignore my body’s signals to slow down before menstruation when progesterone calls for rest. In addition, I had been dealing with endometriosis symptoms since I was a teenager. I was determined not to let them interfere with my life trajectory and learned to ‘push through’ and ignore my symptoms, which I have now learned only exacerbates the inflammation response.
But somewhere within me, I knew something was misaligned. A whisper of resistance to the push became a scream. But I hushed the whisper and oppressed the scream, believing they were weak thoughts I must override.
I forged on against the grain of my biology, and my biology said NO.
At the age of 24, endometriosis became debilitating. It forced me to stop, again, and reflect on my behaviour and priorities.
On paper, my lifestyle should support a high quality of health and vitality. Since I was a teenager I followed a clean whole-food diet with supplementation, intermittent fasting, daily exercise and yoga, a regular sleeping schedule, loving and supportive friends and family, and weekly sauna/ice bath sessions. The list goes on.
However, for a long time, I did not understand just how significantly the requirements for female health differ form than male health because of the cycling nature of our hormones. I had optimized my life according to the male guidelines for health because, until recently, most studies have been male-dominated and rarely mentioned adaptions to suit female biology.
At some point in my research, I stumbled upon Dr Mindy Pelz and Dr Patrick Flynn, who both highlight the nuances of the female hormonal cycle in their work, and that’s when everything started clicking together.
The mystery of my disease and stubborn estrogen dominance became less mysterious.
I know I am not responsible for the disease itself. But I acknowledge that my behavioural patterns have likely contributed somewhat to the severity of my symptoms.
And when navigating a disease that has no cure and that I have little control over, this realization gave me a sense of power. Because my behavioural patterns are something I can control.
It has been HARD for me to let go of discipline.
It rubs against the programming of the modern Western world, which values material success, progress, aesthetic beauty, global recognition, and financial gain.
And I have not let it go completely. It is part of my make-up, to a degree, and still serves me. But I have learned when to use it, and when to let it go.
Since surrendering to my body’s demands instead of those posed upon me from social and personal expectations, and adapting my life to support my cycle, it has begun to heal. (Alongside serious medical intervention)
I thought I was listening to my body by making consistent and disciplined health-related and work-related decisions each day.
But I have learned that truly listening to the body is a very malleable endeavour. It commands adaptability, and perhaps, a more traditionally feminine approach to life.
I have learned to be gentle with myself and stop listening to the voice that says I should be doing more when my body says; slow down.
I have learned to move more meditatively through the world and let go of the pressure to always be achieving something.
I have learned to utilize the periods of my cycle when I feel vital, energized, and creative, and nurture myself when I feel fatigued and low-energy in order to recharge the battery.
Stillness and silence have become more valuable to me the more I honor them.
I have learned that often, true and lasting riches come from reclaiming our energy from external investments and turning our attention to the vitality within.
*Disclaimer, I am not a medical professional. I am only sharing what I have learned from other medical professionals over a decade of trying to understand this disease, and my own speculative links between possible shared psychological, sociological, and physiological tendencies among women with endometriosis — with the acknowledgment that every woman and case is different.